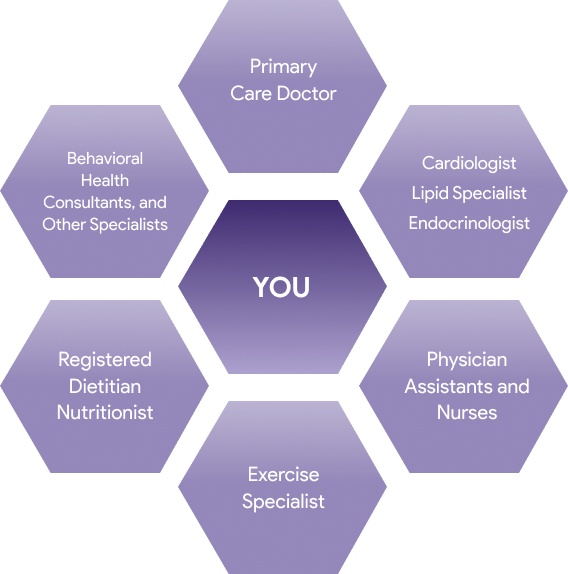
You and your healthcare team27-30
People who actively work with their healthcare team to make treatment decisions have better health results than people who don’t.31 Work with your healthcare professional to:
- Make sure they know everything they need to know about you.
- Come up with a treatment plan that works best for you and matches your preferences, values, and budget.
- Track and manage your progress. That includes a lot more than just triglyceride levels. It also includes:
- Making lifestyle changes and other treatments as convenient as possible for you and your family.
- Finding ways to keep you motivated and satisfied with your treatment plan.
- Making sure your treatment plan is compatible with any other medical conditions you may have.
- Preventing as much as possible the negative effects of high triglycerides, and also preventing or minimizing side effects of treatment.
A key goal of this website and its linked resources is to help you actively participate with your healthcare team in making decisions about how to treat your sHTG.


